One straightforward approach is to think of the infrastructure as being supported by three primary pillars: coding, coverage, and reimbursement. By understanding these areas and how they interact with one another, labs can more efficiently navigate the process of establishing proper coding and reimbursement for their new tests.
MORE: How to Establish Coding and Get Paid for New Lab Tests (On-Demand Free Webinar)
The Importance of proactive engagement with payers
When introducing new lab tests, it is crucial to engage with payers proactively rather than waiting for denials. Many labs make the mistake of assuming that having a test supported by physicians and scientific studies will automatically lead to favorable payer responses. However, the reality is payers often question the value and utility of new tests. To avoid arguing to prove your impact long after a test is in use, labs should establish common ground with payers by aligning their strategy with payer objectives and demonstrating how a new test supports desired outcomes for the payer’s membership.
Proactive engagement involves reaching out to payers early in the test development and validation process, seeking their input, and understanding their coverage policies. By involving payers in the process, labs can address potential concerns and ensure that their test meets the necessary criteria for coverage and reimbursement. This approach not only increases the chances of obtaining favorable reimbursement, but also establishes a collaborative relationship with payers.
Misconceptions about coding and coverage

Ann Lambrix, VP of RCM Consulting, LLS
One common misconception is that coding alone guarantees reimbursement for diagnostic tests. However, coding merely ensures that claims are processed by a payer’s administrative systems. It does not guarantee payment. Labs should primarily be focused on receiving coverage, alongside coding, as their ultimate goal. Simply having an established Common Procedural Terminology (CPT) or Proprietary Lab Analysis (PLA) code does not automatically translate to reimbursement.
“Labs must understand that reimbursement does not equal coverage and that they need to focus on building a case for medical necessity and demonstrating value to payers,” says Ann Lambrix, VP of RCM Solutions for Lighthouse Lab Services.
To secure coverage, labs typically must provide robust evidence demonstrating the clinical utility and cost-effectiveness of their test. This involves conducting well-designed studies, collecting data on patient outcomes, and presenting compelling evidence to payers. Labs should also be prepared to engage in discussions with payers to address any coverage-related questions or concerns. By emphasizing the medical necessity and value of their test, labs can increase the likelihood of obtaining coverage and subsequent reimbursement.
Coverage is the holy grail of reimbursement, says Lena Chaihorsky, Co-Founder and VP of Payer Innovation for Alva10, as it determines whether a test is a covered benefit. Once coverage is obtained, reimbursement comes into play, which involves working with payers to attach a price to the covered benefit.
Understanding coding
CMS sets the baseline rates for Medicare and influences State Medicaid fee schedules. Commercial insurance companies usually negotiate payment based on a percentage of what CMS pays, although it is possible to work with private payers before approaching CMS. Reimbursement is primarily tracked through two code systems: CPT codes and PLA codes. While both coding sets are overseen by the American Medical Association (AMA) and CMS, PLA codes offer a sometimes faster alternative and less rigorous requirements for obtaining reimbursement for proprietary lab tests. However, they are not always recognized by Medicaid or private payers.
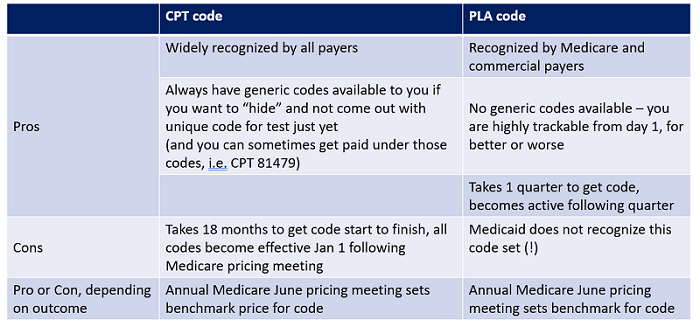
Credit: Alva10, Lena Chaihorsky
Labs can obtain a CPT code by applying to the AMA and meeting a rigorous set of requirements, including providing at least three peer-reviewed papers and demonstrating that the test is in “widespread use” in the US. Alternatively, laboratories can also seek to utilize existing CPT codes if their test aligns with the descriptor and reimbursement rate. The ubiquity of the code set means CPT codes are recognized across most payers.
PLA codes were introduced to cover Advanced Diagnostic Lab Tests (ADLTs) and Clinical Diagnostic Lab Tests (CDLTs), offering a detailed description of a unique lab analysis. Labs can obtain PLA codes by applying through the AMA under a less strict set of requirements, including that the test is “available for ordering by physicians.” However, reimbursement for the test must be established by Medicare. PLA codes offer increased trackability but often require prior authorization to receive reimbursement from private payers.
It’s always advisable to consult an expert when determining the best reimbursement and coding pathway for any new test your lab develops.
Recognizing payers as customers
Labs should remember they have multiple customers to consider when developing a new diagnostic test. While clinicians play a crucial role in ordering tests, insurance companies serve as the economic customers of the industry since they reimburse labs for their services. This means labs need to shift their perspective and consider the strategic goals of their payers when developing products. By building tools and products that align with insurance companies’ spending objectives and population goals, labs can increase their chances of obtaining reimbursement.
While each network will have different goals and benchmarks, most are focused on managing costs while ensuring quality patient care. Labs should design their tests with these factors in mind, aiming to provide meaningful clinical information at an affordable cost. By demonstrating how their tests can contribute to cost savings, improved patient outcomes, and more effective treatment decisions, labs can position themselves as valuable partners to payers and establish consistent reimbursement for their tests.
Looking ahead
Labs must take a proactive approach in engaging with payers, recognizing that coding is not sufficient for reimbursement, and understanding the importance of coverage as part of a comprehensive reimbursement strategy. By aligning tests with the objectives of payers and demonstrating value, labs can improve their chances of obtaining reimbursement upfront for diagnostic tests.
If you’re seeking to establish coding and reimbursement for a new test, or tighten your overall revenue cycle management, our in-house consultants are available to assist you. Contact us today for a free consultation.

Trackbacks/Pingbacks